When navigating the world of healthcare, numerous terms and processes can be overwhelming. One such document that plays a crucial role in ensuring patients receive the necessary treatment is the Letter of Medical Necessity (LMN).
What Is A Letter Of Medical Necessity?
A letter of medical necessity, often abbreviated as LMN, is a document that outlines why a specific treatment, service, or item is essential for a patient’s health. It serves as justification for insurance coverage or other benefits by providing a physician’s clinical reasoning for the prescribed treatment. The LMN helps to demonstrate the medical necessity of the prescribed intervention, ensuring that patients receive the appropriate care for their diagnosed condition.
What Is The Purpose Of A Letter Of Medical Necessity?
1. Evidence-Based Justification
One of the key purposes of an LMN is to provide evidence-based justification for the prescribed treatment. By referencing medical literature, clinical guidelines, and expert opinions, the LMN establishes a strong rationale for why the recommended intervention is essential for the patient’s health. This evidence-based approach not only enhances the credibility of the document but also increases the likelihood of approval for insurance coverage or other benefits.
2. Facilitating Communication and Coordination
Another purpose of a letter of medical necessity is to facilitate communication and coordination among healthcare providers, insurance companies, and other stakeholders involved in the patient’s care. By clearly articulating the medical need for a specific treatment, the LMN ensures that all parties are aligned regarding the recommended intervention and its importance in managing the patient’s condition. This communication helps streamline the approval process and promotes collaborative decision-making in healthcare.
3. Advocating for Patient Rights
Additionally, an LMN serves as a tool for advocating for patient rights and ensuring access to necessary healthcare services. By detailing the medical necessity of a treatment or service, the LMN empowers patients to receive the care they need to improve their health outcomes. This advocacy not only benefits individual patients but also contributes to advancing healthcare equity and quality of care across diverse populations.
Difference Between A Letter Of Medical Necessity And A Prescription
It is essential to distinguish between a letter of medical necessity and a prescription, as they serve different purposes in the healthcare setting. While a prescription is a written directive from a healthcare provider for a specific medication or treatment, a letter of medical necessity provides a detailed explanation of why a particular intervention is medically necessary. The LMN serves as a supporting document that justifies the need for the prescribed treatment, helping ensure that patients receive the appropriate care for their condition.
What Are Some Items That Require A Letter Of Medical Necessity?
Various items and services may require a letter of medical necessity to justify their medical necessity. Some common examples include:
1. Durable Medical Equipment (DME)
Durable Medical Equipment (DME) such as wheelchairs, walkers, and hospital beds may require an LMN to demonstrate their necessity for a patient’s health. The LMN for DME would detail the patient’s mobility limitations, functional needs, and the recommended equipment to support their daily living activities. By outlining the medical necessity of the DME, the LMN helps ensure that patients receive the appropriate assistive devices to enhance their quality of life.
2. Medical Procedures
Certain medical procedures, such as surgeries or specialized treatments, may necessitate a letter of medical necessity to explain the clinical rationale behind the intervention. For example, a patient requiring a diagnostic procedure to evaluate a suspected medical condition would need an LMN outlining the diagnostic criteria, risks, benefits, and expected outcomes of the procedure. The LMN for medical procedures helps ensure that patients undergo necessary interventions based on sound medical judgment and evidence-based practice.
3. Therapeutic Services
Therapies such as physical therapy, occupational therapy, or speech therapy may require an LMN to justify their importance in a patient’s treatment plan. The LMN for therapeutic services would outline the patient’s therapy goals, functional limitations, and the recommended frequency and duration of therapy sessions. By detailing the medical necessity of therapeutic services, the LMN supports the patient’s rehabilitation, functional improvement, and overall well-being through evidence-based interventions.
4. Prescription Medications
In some cases, prescription medications may require a letter of medical necessity to explain why a specific drug is necessary for a patient’s health. For instance, a patient with a rare medical condition requiring a specialized medication would need an LMN detailing the diagnosis, treatment history, and the rationale for the prescribed drug. The LMN for prescription medications ensures that patients have access to the necessary pharmacotherapy to manage their condition effectively and improve their quality of life.
When May You Need A Letter Of Medical Necessity?
You may need a letter of medical necessity in various situations where it is necessary to justify the medical need for a specific treatment, service, or item. Some common scenarios where an LMN may be required include:
1. Insurance Coverage
When seeking insurance coverage for a particular treatment or service, an LMN may be necessary to demonstrate the medical necessity of the prescribed intervention. Insurance companies often require a detailed explanation of why the recommended treatment is essential for the patient’s health to approve coverage and reimbursement. The LMN plays a critical role in advocating for insurance approval by providing a thorough rationale for the prescribed intervention.
2. Authorization for Services
Healthcare providers may require a letter of medical necessity to authorize certain services or procedures for a patient’s care. Prior authorization processes often involve submitting an LMN that justifies the medical need for the recommended intervention, ensuring that services are approved based on clinical necessity. The LMN helps streamline the authorization process by providing a comprehensive explanation of why the prescribed treatment is essential for the patient’s health.
3. Appealing Denials
If an insurance claim is denied due to a lack of medical necessity or insufficient documentation, a well-drafted LMN can be instrumental in appealing the decision. By submitting a detailed letter of medical necessity that addresses the reasons for the denial and provides additional clinical evidence, patients and healthcare providers can advocate for the approval of the recommended treatment. The LMN serves as a persuasive tool in appealing denials and securing coverage for essential healthcare services.
How To Get A Letter Of Medical Necessity
Obtaining a letter of medical necessity typically involves working closely with your healthcare provider to ensure that all relevant information is included in the document. To get an LMN, follow these steps:
Step 1: Schedule an Appointment
Schedule an appointment with your healthcare provider to discuss the need for a letter of medical necessity. During the appointment, communicate the treatment, service, or item for which you require the LMN and provide any relevant medical records or documentation to support your request.
Step 2: Provide Detailed Information
Provide your healthcare provider with detailed information about your medical condition, treatment history, current symptoms, and any previous interventions you have undergone. Be prepared to discuss the reasons why you believe the prescribed treatment is necessary for managing your health.
Step 3: Collaborate on Drafting the LMN
Work collaboratively with your healthcare provider to draft a comprehensive letter of medical necessity that outlines the clinical rationale for the prescribed intervention. Ensure that the LMN includes all necessary components, such as your diagnosis, treatment plan, expected outcomes, and provider information.
Step 4: Review and Finalize
Review the letter of medical necessity for accuracy, completeness, and clarity before submitting it to the appropriate party, such as your insurance company or healthcare facility. Make sure that all information is up to date, relevant to your medical condition, and aligns with the requirements for medical necessity justification.
Step 5: Follow Up
After submitting the LMN, follow up with the relevant party to ensure that the document has been received and is being processed. Stay engaged in the approval process, provide any additional information or documentation as needed, and advocate for the timely review and decision on the medical necessity request.
How Long Is An LMN Valid?
The validity of a letter of medical necessity may vary depending on the specific requirements of the insurance provider or healthcare facility. In general, an LMN is typically valid for a specified period, after which it may need to be updated or renewed to continue justifying the medical necessity of a treatment or service. It is essential to check with the relevant parties to determine the validity period of an LMN and ensure that it remains up to date to support your healthcare needs.
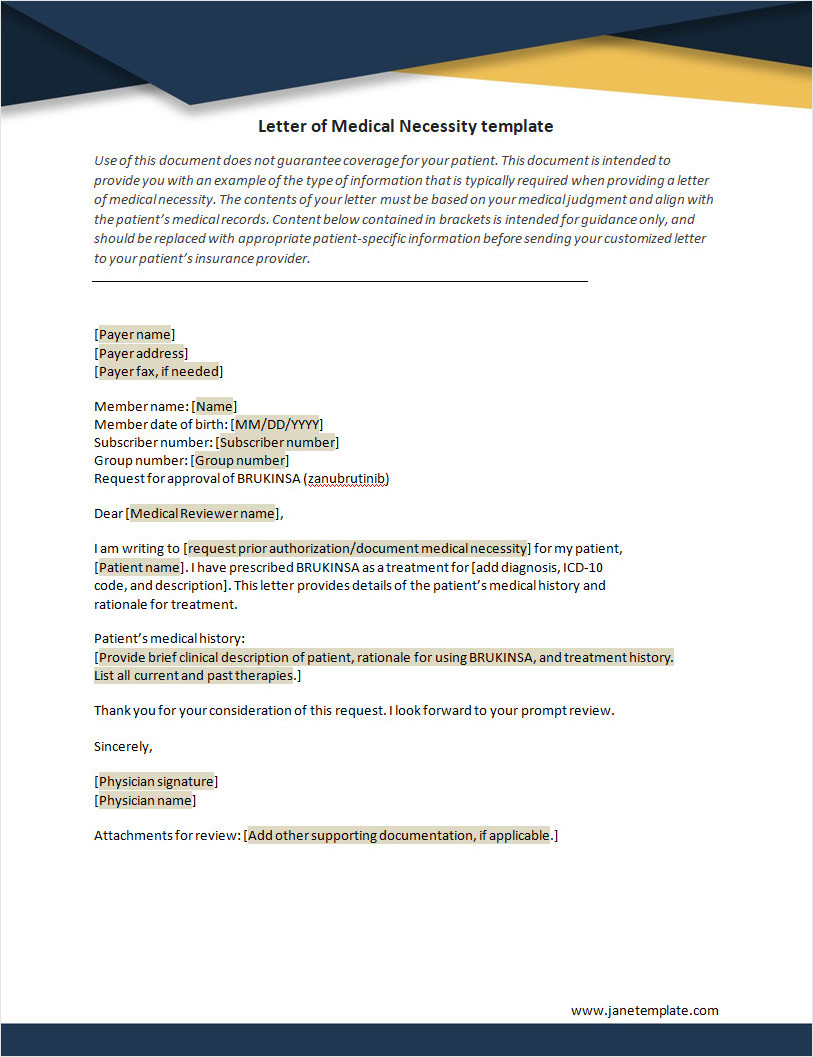
Letter of Medical Necessity Template
Start using our free letter of medical necessity template today to support insurance claims, justify treatment plans, and ensure patients receive the care they need.
Letter of Medical Necessity Template – Download